| Degrees | Symptoms | Symptoms Nocturnes | DEMI |
| 1 - Intermittent | <1 time / week or asymptomatic; DEMI; normal between attacks. | ≤ 2 per month | ≥ 80% predicted Variability<20% |
| 2 - Mild persistent | ≥ 1 per week | > 2 per month | ≥ 80% predicted Variability 20-30% |
| 3 - Moderate persistent | Daily; Uses Bronchodilators short daily action; Crises affect activity. | > 1 per week | ≥ 60% - <80% predicted Variability> 30% |
| 4 - Record | Constants; Activity limitedphysical | Frequent (almost daily) | ≤ 60% predicted Variability> 30% |

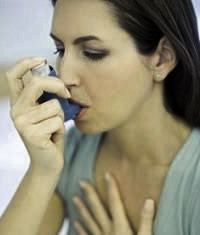
Asthma is a chronic inflammatory condition of the airways, causes of which are not completely understood. As a result of inflammation airway becomes narrow-reactive and easily responsive to various stimuli. This can result in coughing, wheezing, chest tightness and breathlessness, which are most common symptoms at night. The narrowing of the airways is usually reversible, but in patients with chronic asthma, the inflammation can determine irreversible airflow obstruction. The pathological features include the presence of inflammatory cells in the airways, plasma exudation, edema, muscle hypertrophy, mucus plugs and epithelial desquamation.


